Clostridium difficile infection.
Leffler DA, Lamont JT.
N Engl J Med. 2015 Apr 16;372(16):1539-48. doi: 10.1056/NEJMra1403772.
Clostridium difficile is an anaerobic gram-positive, spore-forming, toxin-producing bacillus that is transmitted among humans through the fecal–oral route. The relationship between the bacillus and humans was once thought to be commensal,1 but C. difficile has emerged as a major enteric pathogen with worldwide distribution. In the United States, C. difficile is the most frequently reported nosocomial pathogen. A surveillance study in 2011 identified 453,000 cases of C. difficile infection and 29,000 deaths associated with C. difficile infection; approximately a quarter of those infections were community-acquired.2 Nosocomial C. difficile infection more than quadruples the cost of hospitalizations,3 increasing annual expenditures by approximately $1.5 billion in the United States.4 In this article, we review the changing epidemiology of this infection, discuss risk factors and preventive strategies, outline current recommendations for treatment, and highlight developing strategies for disease control.
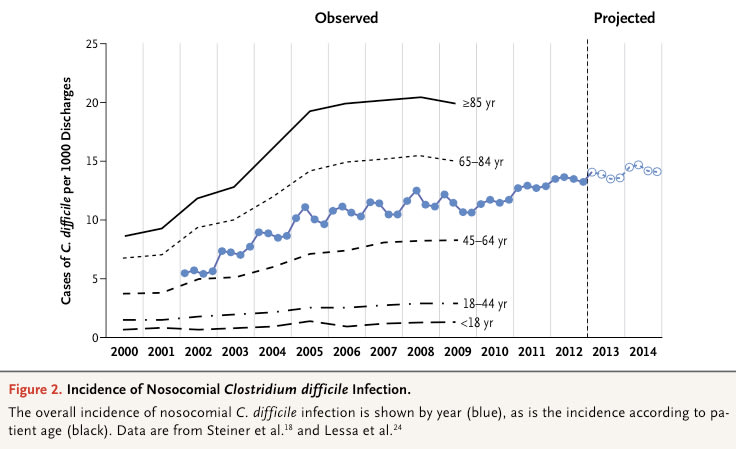


Figure 3. Rates of Cure and Changes to the Microbiota after Fecal Microbial Transplantation for Recurrent Clostridium difficile Infection.
Among patients with recurrent C. difficile infection, the rate of cure without relapse was higher among those who received an infusion of donor feces than among those who received vancomycin with or without bowel lavage (Panel A). Fecal microbial diversity in recipients before and after the infusion of donor feces is compared with the diversity in healthy donors (Panel B). Microbial diversity is expressed by Simpson’s Reciprocal Index. The index ranges from 1 to 250, with higher values indicating more diversity. The box- and-whisker plots indicate interquartile ranges (boxes), medians (dark hori- zontal lines in the boxes), and highest and lowest values (whiskers above and below the boxes).
van Nood E, Vrieze A, Nieuwdorp M, et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med 2013;368:407-15.
Leffler DA, Lamont JT.
N Engl J Med. 2015 Apr 16;372(16):1539-48. doi: 10.1056/NEJMra1403772.
Clostridium difficile is an anaerobic gram-positive, spore-forming, toxin-producing bacillus that is transmitted among humans through the fecal–oral route. The relationship between the bacillus and humans was once thought to be commensal,1 but C. difficile has emerged as a major enteric pathogen with worldwide distribution. In the United States, C. difficile is the most frequently reported nosocomial pathogen. A surveillance study in 2011 identified 453,000 cases of C. difficile infection and 29,000 deaths associated with C. difficile infection; approximately a quarter of those infections were community-acquired.2 Nosocomial C. difficile infection more than quadruples the cost of hospitalizations,3 increasing annual expenditures by approximately $1.5 billion in the United States.4 In this article, we review the changing epidemiology of this infection, discuss risk factors and preventive strategies, outline current recommendations for treatment, and highlight developing strategies for disease control.
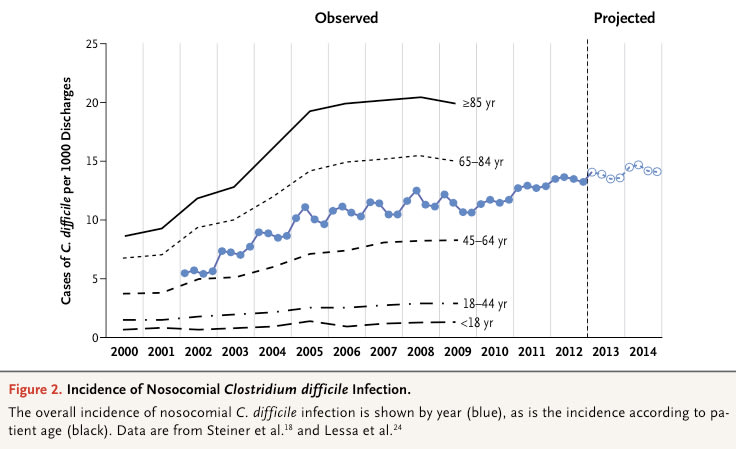


Figure 3. Rates of Cure and Changes to the Microbiota after Fecal Microbial Transplantation for Recurrent Clostridium difficile Infection.
Among patients with recurrent C. difficile infection, the rate of cure without relapse was higher among those who received an infusion of donor feces than among those who received vancomycin with or without bowel lavage (Panel A). Fecal microbial diversity in recipients before and after the infusion of donor feces is compared with the diversity in healthy donors (Panel B). Microbial diversity is expressed by Simpson’s Reciprocal Index. The index ranges from 1 to 250, with higher values indicating more diversity. The box- and-whisker plots indicate interquartile ranges (boxes), medians (dark hori- zontal lines in the boxes), and highest and lowest values (whiskers above and below the boxes).
van Nood E, Vrieze A, Nieuwdorp M, et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med 2013;368:407-15.