総説 リゾフォスファチジル酸 LPAと炎症
You have free access to this contentLysophosphatidic acid in atherosclerotic diseases (pages 465–482)
Andreas Schober and Wolfgang Siess
Lysophosphatidic acid (LPA) is a potent bioactive phospholipid. As many other biological active lipids, LPA is an autacoid: it is formed locally on demand, and it acts locally near its site of synthesis. LPA has a plethora of biological activities on blood cells (platelets, monocytes) and cells of the vessel wall (endothelial cells, smooth muscle cells, macrophages) that are all key players in atherosclerotic and atherothrombotic processes. The specific cellular actions of LPA are determined by its multifaceted molecular structures, the expression of multiple G-protein coupled LPA receptors at the cell surface and their diverse coupling to intracellular signalling pathways. Numerous studies have now shown that LPA has thrombogenic and atherogenic actions. Here, we aim to provide a comprehensive, yet concise, thoughtful and critical review of this exciting research area and to pinpoint potential pharmacological targets for inhibiting thrombogenic and atherogenic activities of LPA. We hope that the review will serve to accelerate knowledge of basic and clinical science, and to foster drug development in the field of LPA and atherosclerotic/atherothrombotic diseases.
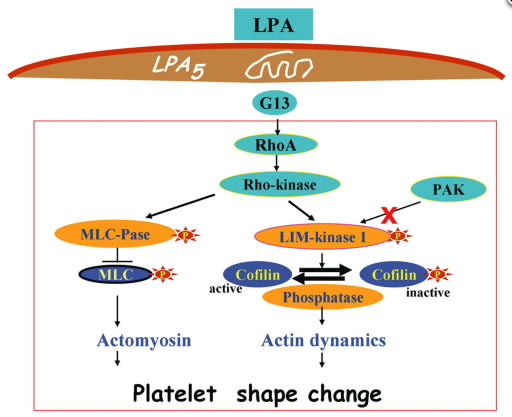
LPA-induced platelet signalling during platelet shape change:理解されている血小板内細胞内情報伝達レベル
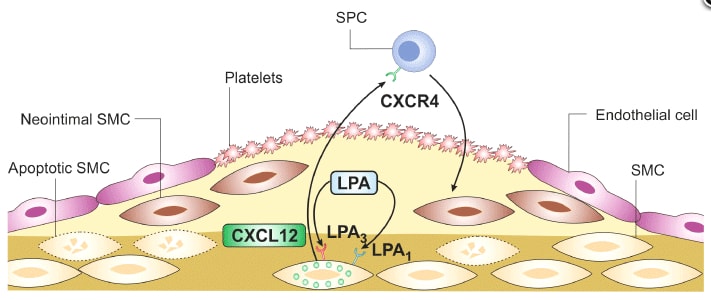
LPA induces neointima formation after vascular injury:理解されている血管新生メカニズム
原著
1.関節炎マウスの大動脈はセロトニンによる収縮反応が悪い「炎症」と「再生」
Contractile, but not endothelial, dysfunction in early inflammatory arthritis: a possible role for matrix metalloproteinase-9 (pages 505–514)
SL Reynolds, AS Williams, H Williams, S Smale, HJ Stephenson, N Amos, SJ George, VB O'Donnell and D Lang
BACKGROUND AND PURPOSE Excess morbidity/mortality in rheumatoid arthritis (RA) is associated with increased incidence of cardiovascular disease. In this ‘proof-of-concept’ study, vascular function was characterized in the murine collagen-induced arthritis (mCIA) model, the benchmark choice for evaluation of the pathological processes and assessment of new therapies.
EXPERIMENTAL APPROACH Mice in the very early stages of arthritis development [and appropriate naïve (non-immunized) age-matched controls] were used in the study. Blood pressure was measured using tail cuff plethysmography. Vascular function in rings of isolated aorta was studied with isometric tension myography. Levels of NO metabolites (NOx), MMP-9 protein and IL-1β in plasma and MMP-9 protein in aortic homogenates were quantified.
KEY RESULTS Impaired vascular contractile responses in arthritis were unaffected by ex vivo inhibition of NOS (endothelial/neuronal and inducible) or COX activities. Endothelium-dependent and -independent relaxation, plasma NOx and blood pressure were unaffected by arthritis. Plasma and aortic homogenate MMP-9 protein levels were increased significantly in arthritis. Incubation of aortic tissues from naïve control animals with exogenous MMP-9 impaired subsequent contractile responses, mirroring that observed in arthritis. A role for IL-1β in perpetuating contractile dysfunction and increasing aortic MMP-9 was excluded.
CONCLUSIONS AND IMPLICATIONS These data identify for the first time a relationship between early arthritis and contractile dysfunction and a possible role for MMP-9 therein, in the absence of overt endothelial dysfunction or increased NO production. As such, MMP-9 may constitute a significant target for early intervention in RA patients with a view to decreasing risk of cardiovascular disease.
炎症期にIL-1β,回復期にMMP9の発現により,セロトニンの収縮反応が低下するという,タイムコース評価の難しい研究系です。
2.Epithelium-dependent modulation of responsiveness of airways from caveolin-1 knockout mice is mediated through cyclooxygenase-2 and 5-lipoxygenase (pages 548–560)
Pawan Sharma, Min H Ryu, Sujata Basu, Sarah A Maltby, Behzad Yeganeh, Mark M Mutawe, Richard W Mitchell and Andrew J Halayko
epartment of Internal Medicine, University of Manitoba, Winnipeg, MB, Canada

BACKGROUND AND PURPOSE Acute silencing of caveolin-1 (Cav-1) modulates receptor-mediated contraction of airway smooth muscle. Moreover, COX-2- and 5-lipoxygenase (5-LO)-derived prostaglandin and leukotriene biosynthesis can influence smooth muscle reactivity. COX-2 half-life can be prolonged through association with Cav-1. We suggested that lack of Cav-1 modulated levels of COX-2 which in turn modulated tracheal contraction, when arachidonic acid signalling was disturbed by inhibition of COX-2.
EXPERIMENTAL APPROACH Using tracheal rings from Cav-1 knockout (KO) and wild-type mice (B6129SF2/J), we measured isometric contractions to methacholine and used PCR, immunoblotting and immunohistology to monitor expression of relevant proteins.
KEY RESULTS Tracheal rings from Cav-1 KO and wild-type mice exhibited similar responses, but the COX-2 inhibitor, indomethacin, increased responses of tracheal rings from Cav-1 KO mice to methacholine. The phospholipase A2 inhibitor, eicosatetraynoic acid, which inhibits formation of both COX-2 and 5-LO metabolites, had no effect on wild-type or Cav-1 KO tissues. Indomethacin-mediated hyperreactivity was ablated by the LTD4 receptor antagonist (montelukast) and 5-LO inhibitor (zileuton). The potentiating effect of indomethacin on Cav-1 KO responses to methacholine was blocked by epithelial denudation. Immunoprecipitation showed that COX-2 binds Cav-1 in wild-type lungs. Immunoblotting and qPCR revealed elevated levels of COX-2 and 5-LO protein, but not COX-1, in Cav-1 KO tracheas, a feature that was prevented by removal of the epithelium.
CONCLUSION AND IMPLICATIONS The indomethacin-induced hypercontractility observed in Cav-1 KO tracheas was linked to increased expression of COX-2 and 5-LO, which probably enhanced arachidonic acid shunting and generation of pro-contractile leukotrienes when COX-2 was inhibited.
3.アデノシンに似ているコルディセピン
Blockade of adipocyte differentiation by cordycepin (pages 561–575)
Shuhei Takahashi, Minori Tamai, Shotaro Nakajima, Hironori Kato, Hisashi Johno, Tomoyuki Nakamura and Masanori Kitamura
BACKGROUND AND PURPOSE Cordyceps militaris has the potential to suppress differentiation of pre-adipocytes. However, the active entities in the extract and the underlying mechanisms of its action are not known. Hence, we investigated whether and how cordycepin (3′-deoxyadenosine), a constituent of C. militaris, inhibits adipogenesis.
EXPERIMENTAL APPROACH Differentiation of 3T3-L1 pre-adipocytes and pre-adipocytes in primary cultures was induced by Insulin, dexamethasone and IBMX, and these were used as in vitro models of adipogenesis. The effects of cordycepin on adipogenesis were examined with particular focus on the regulation of CCAAT/enhancer-binding protein β (C/EBPβ) and PPARγ.
KEY RESULTS Cordycepin suppressed the lipid accumulation and induction of adipogenic markers that occurred on differentiation of pre-adipocytes and also blocked the down-regulation of a pre-adipocyte marker. This anti-adipogenic effect was reversible and mediated by an adenosine transporter, but not A1, A2 or A3 adenosine receptors. This effect of cordycepin was not reproduced by other adenosine-related substances, including ATP, ADP and adenosine. Early induction of the adipogenic C/EBPβ–PPARγ pathway was suppressed by cordycepin. Blockade of mTORC1 via inhibition of PKB (Akt) and activation of AMP kinase was identified as the crucial upstream event targeted by cordycepin. In addition to its negative effect on adipogenesis, cordycepin suppressed lipid accumulation in mature adipocytes.
CONCLUSIONS AND IMPLICATIONS These results suggest that the anti-adipogenic effects of cordycepin occur through its intervention in the mTORC1-C/EBPβ–PPARγ pathway. Cordycepin, by blocking both adipogenesis and lipid accumulation, may have potential as a therapeutic agent for effective treatment of obesity and obesity-related disorders.
mTOR複合体1への作用が重要
1)コルディセピンは,「さなぎ」に含まれています。「さなぎ」の粉末は,腸粘膜新生を抑制,がん細胞増殖を抑制などの作用があるとされています。
2)PKB活性を阻害する可能性があり,mTORC1を抑制する作用があります。
3)コルディセピンは,C/EBP mRNAを低下させる可能性があります。
4.Toll-like receptor 4 knockout protects against anthrax lethal toxin-induced cardiac contractile dysfunction: role of autophagy (pages 612–626)
Machender R Kandadi, Arthur E Frankel and Jun Ren 競合する研究内容
BACKGROUND AND PURPOSE Anthrax lethal toxin (LeTx) is known to induce circulatory shock and death, although the underlying mechanisms have not been elucidated. This study was designed to evaluate the role of toll-like receptor 4 (TLR4) in anthrax lethal toxin-induced cardiac contractile dysfunction.
EXPERIMENTAL APPROACH Wild-type (WT) and TLR4 knockout (TLR-/-) mice were challenged with lethal toxin (2 µg·g-1, i.p.), and cardiac function was assessed 18 h later using echocardiography and edge detection. Small interfering RNA (siRNA) was employed to knockdown TLR4 receptor or class III PI3K in H9C2 myoblasts. GFP–LC3 puncta was used to assess autophagosome formation. Western blot analysis was performed to evaluate autophagy (LC3, Becline-1, Agt5 and Agt7) and endoplasmic reticulum (ER) stress (BiP, eIF2α and calreticulin).
KEY RESULTS In WT mice, lethal toxin exposure induced cardiac contractile dysfunction, as evidenced by reduced fractional shortening, peak shortening, maximal velocity of shortening/re-lengthening, prolonged re-lengthening duration and intracellular Ca2+ derangement. These effects were significantly attenuated or absent in the TLR4 knockout mice. In addition, lethal toxin elicited autophagy in the absence of change in ER stress. Knockdown of TLR4 or class III PI3 kinase using siRNA but not the autophagy inhibitor 3-methyladenine significantly attenuated or inhibited lethal toxin-induced autophagy in H9C2 cells.
CONCLUSION AND IMPLICATIONS Our results suggest that TLR4 may be pivotal in mediating the lethal cardiac toxicity induced by anthrax possibly through induction of autophagy. These findings suggest that compounds that negatively modulate TLR4 signalling and autophagy could be used to treat anthrax infection-induced cardiovascular complications.
主催:一般社団法人 日本集中治療医学会


日 時:平成24年(2012年) 9月22日(土曜日) 16:00~18:00
会 場:ベルサール九段 ROOM3(4階)
〒102-0073 東京都千代田区九段北1-8-10住友不動産九段ビル
16:00~16:05 開会挨拶(司会)
丸藤 哲(北海道大学医学研究科侵襲制御医学講座救急医学分野 教授)
16:05~16:25 敗血症とは
藤島 清太郎(慶應義塾大学病院救急部 准教授)
16:25~16:45 敗血症の疫学
松田 直之(名古屋大学大学院医学系研究科 救急集中治療医学 教授)
16:45~17:05 日本版敗血症診療ガイドラインの意義
織田 成人(千葉大学大学院医学研究院救急集中治療医学 教授)
17:05~17:25 敗血症の予後を2020年までに改善させるためには
藤谷 茂樹(東京ベイ浦安市川医療センター センター長)
17:25~17:55 マスコミ記者会見
17:55~18:00 閉会挨拶
氏家 良人(岡山大学大学院医歯薬学総合研究科救急医学 教授)
Surviving Sepsis Campaign Guidelines 公表後の補足データ
Chest. 2011 Nov;140(5):1223-31.
Nationwide trends of severe sepsis in the 21st century (2000-2007).
Kumar G, Kumar N, Taneja A, Kaleekal T, Tarima S, McGinley E, Jimenez E, Mohan A, Khan RA, Whittle J, Jacobs E, Nanchal R; Milwaukee Initiative in Critical Care Outcomes Research Group of Investigators.
Source
Department of Medicine, Division of Pulmonary and Critical Care, Medical College of Wisconsin, 9200 W Wisconsin Ave, Milwaukee, WI 53226, USA.
Abstract
BACKGROUND:
Severe sepsis is common and often fatal. The expanding armamentarium of evidence-based therapies has improved the outcomes of persons with this disease. However, the existing national estimates of the frequency and outcomes of severe sepsis were made before many of the recent therapeutic advances. Therefore, it is important to study the outcomes of this disease in an aging US population with rising comorbidities.
METHODS:
We used the Healthcare Costs and Utilization Project's Nationwide Inpatient Sample (NIS) to estimate the frequency and outcomes of severe sepsis hospitalizations between 2000 and 2007. We identified hospitalizations for severe sepsis using International Classification of Diseases, Ninth Revision, Clinical Modification codes indicating the presence of sepsis and organ system failure. Using weights from NIS, we estimated the number of hospitalizations for severe sepsis in each year. We combined these with census data to determine the number of severe sepsis hospitalizations per 100,000 persons. We used discharge status to identify in-hospital mortality and compared mortality rates in 2000 with those in 2007 after adjusting for demographics, number of organ systems failing, and presence of comorbid conditions.
RESULTS:
The number of severe sepsis hospitalizations per 100,000 persons increased from 143 in 2000 to 343 in 2007. The mean number of organ system failures during admission increased from 1.6 to 1.9 (P < .001). The mean length of hospital stay decreased from 17.3 to 14.9 days. The mortality rate decreased from 39% to 27%. However, more admissions ended with discharge to a long-term care facility in 2007 than in 2000 (35% vs 27%, P < .001).
CONCLUSIONS:
An increasing number of admissions for severe sepsis combined with declining mortality rates contribute to more individuals surviving to hospital discharge. Importantly, this leads to more survivors being discharged to skilled nursing facilities and home with in-home care. Increased attention to this phenomenon is warranted.
1. PM10による肺炎症に対するロバスタチンの抑制効果;Urban air PM10 (EHC-93) from Environmental Health Directorate, Health Canada (Ottawa, ON, Canada)
Ryohei Miyata, Ni Bai, Renaud Vincent, Don D. Sin, and Stephan F. Van Eeden
Novel properties of statins: suppression of the systemic and bone marrow responses induced by exposure to ambient particulate matter (PM10) air pollution
Am J Physiol Lung Cell Mol Physiol September 15, 2012 303:L492-L499

Stephanus (Stephan) F. van Eeden MD, PhD, FRCPC(C)
Department of Internal Medicine, University of British Columbia
Abstract
Exposure to ambient particulate matter (PM10) elicits systemic inflammatory responses that include the stimulation of bone marrow and progression of atherosclerosis. The present study was designed to assess the effect of repeated exposure of PM10 on the turnover and release of polymorphonuclear leukocytes (PMNs) from the bone marrow into the circulation and the effect of lovastatin on the PM10-induced bone marrow stimulation. Rabbits exposed to PM10 three times a week for 3 wk, were given a bolus of 5′-bromo-2′-deoxyuridine to label dividing cells in the marrow to calculate the transit time of PMNs in the mitotic or postmitotic pool. PM10 exposure accelerated the turnover of PMNs by shortening their transit time through the marrow (64.8 ± 1.9 h vs. 34.3 ± 7.4 h, P < 0.001, control vs. PM10). This was predominantly due to a rapid transit of PMNs through the postmitotic pool (47.9 ± 0.7 h vs. 21.3 ± 4.3 h, P < 0.001, control vs. PM10) but not through the mitotic pool. Lovastatin delayed the transit time of postmitotic PMNs (38.2 ± 0.5 h, P < 0.001 vs. PM10) and shifted the postmitotic PMN release peak from 30 h to 48 h. PM10 exposure induced the prolonged retention of newly released PMNs in the lung, which was reduced by lovastatin (P < 0.01). PM10 exposure increased plasma interleukin-6 levels with significant reduction by lovastatin (P < 0.01). We conclude that lovastatin downregulates the PM10-induced overactive bone marrow by attenuating PM10.
MANY WELL-DOCUMENTED STUDIES have supported the concept that ambient particulate matter (particles less than 10 μm or PM10) exposure induces systemic inflammatory responses, characterized by an increase in circulating proinflammatory mediators and blood elements such as leukocytes or platelets. These systemic responses to PM10 exposure have been implicated in the risk for downstream cardiovascular events. The focus of their research efforts are the mechanisms of lung inflammation, particularly, lung inflammation caused by infection, cigarette smoking and air pollution.
2. 腸管由来のセロトニンが肺高血圧を緩和している可能性
Shariq Abid, Amal Houssaini, Caroline Chevarin, Elisabeth Marcos, Claire-Marie Tissot, Guillaume Gary-Bobo, Feng Wan, Nathalie Mouraret, Valerie Amsellem, Jean-Luc Dubois-Randé, Michel Hamon, and Serge Adnot
Inhibition of gut- and lung-derived serotonin attenuates pulmonary hypertension in mice
Am J Physiol Lung Cell Mol Physiol September 15, 2012 303:L500-L508

Serge Adnot, MD, PhD
Medical School of Creteil
Hôpital Henri Mondor
Créteil, France
Dr. Adnot is a Professor in the Department of Physiology at the Medical school of Créteil, and Cardiologist and Head of Medical Department of Functional Testing at Hôpital Henri Mondor, and Director of INSERM Research Unit 651 (2005).
Abstract
Decreasing the bioavailability of serotonin (5-HT) by inhibiting its biosynthesis may represent a useful adjunctive treatment of pulmonary hypertension (PH). We assessed this hypothesis using LP533401, which inhibits the rate-limiting enzyme tryptophan hydroxylase 1 (Tph1) expressed in the gut and lung, without inhibiting Tph2 expressed in neurons. Mice treated repeatedly with LP533401 (30–250 mg/kg per day) exhibited marked 5-HT content reductions in the gut, lungs, and blood, but not in the brain. After a single LP533401 dose (250 mg/kg), lung and gut 5-HT contents decreased by 50%, whereas blood 5-HT levels remained unchanged, suggesting gut and lung 5-HT synthesis. Treatment with the 5-HT transporter (5-HTT) inhibitor citalopram decreased 5-HT contents in the blood and lungs but not in the gut. In transgenic SM22-5-HTT+ mice, which overexpress 5-HTT in smooth muscle cells and spontaneously develop PH, 250 mg/kg per day LP533401 or 10 mg/kg per day citalopram for 21 days markedly reduced lung and blood 5-HT levels, right ventricular (RV) systolic pressure, RV hypertrophy, distal pulmonary artery muscularization, and vascular Ki67-positive cells (P < 0.001). Combined treatment with both drugs was more effective in improving PH-related hemodynamic parameters than either drug alone. LP533401 or citalopram treatment partially prevented PH development in wild-type mice exposed to chronic hypoxia. Lung and blood 5-HT levels were lower in hypoxic than in normoxic mice and decreased further after LP533401 or citalopram treatment. These results provide proof of concept that inhibiting Tph1 may represent a new therapeutic strategy for human PH.
Tryptophan Hydroxylase は,セロトニン合成酵素であり,(トリプトファンの5位にヒドロキシル基をふかし,5-ヒドロキシトリプトファン(5-HTP)を形成する。この5-HTPがセロトニン合成の重要な律速酵素となる。Tph1とThp2つのサブタイプが,別々な遺伝子デコードされている。このうち,Thp-1は消化管や肺や精巣に,Thp-2はニューロンに比較的高い特異性を持って存在しているようだ。この研究で用いられているLP533401が,比較的選択性の高いTph1阻害薬である。
3. Alveolar Fluid Clearance (AFC)
Yosaf F. Zeyed, Julie A. Bastarache, Michael A. Matthay, and Lorraine B. Ware
The severity of shock is associated with impaired rates of net alveolar fluid clearance in clinical acute lung injury
Am J Physiol Lung Cell Mol Physiol September 15, 2012 303:L550-L555

Abstract
The rate of alveolar fluid clearance (AFC) is associated with mortality in clinical acute lung injury (ALI). Patients with ALI often develop circulatory shock, but how shock affects the rate of AFC is unknown. To determine the effect of circulatory shock on the rate of AFC in patients with ALI, the rate of net AFC was measured in 116 patients with ALI by serial sampling of pulmonary edema fluid. The primary outcome was the rate of AFC in patients with shock compared with those without shock. We also tested the effects of shock severity and bacteremia. Patients with ALI and shock (n = 86) had significantly slower rates of net AFC compared with those without shock (n = 30, P = 0.03), and AFC decreased significantly as the number of vasopressors increased. Patients with positive blood cultures (n = 21) had slower AFC compared with patients with negative blood cultures (n = 96, P = 0.023). In addition, the edema fluid-to-plasma protein ratio, an index of alveolar-capillary barrier permeability, was highest in patients requiring the most vasopressors (P < 0.05). Patients with ALI complicated by circulatory shock and bacteremia had slower rates of AFC compared with patients without shock or bacteremia. An impaired capacity to reabsorb alveolar edema fluid may contribute to high mortality among patients with sepsis-induced ALI. These findings also suggest that vasopressor use may be a marker of alveolar-capillary barrier permeability in ALI and provide justification for new therapies that enhance alveolar epithelial and endothelial barrier integrity in ALI, particularly in patients with shock.
※ Lorraine B. Wareのエディトリアル
Modeling human lung disease in animals
Am J Physiol Lung Cell Mol Physiol February 2008 294:L149-L150

2012年9月13日(木)第1回World Sepsis Dayとして,AM10:13に4時間ろうそくに点火を行い,4時間の長さを十分に体得して頂きました。遅すぎる敗血症診療を解決することが大切です。そして,敗血症管理におけるGlobal Sepsis Allianceの2020年までの到達目標について,当教室において解説させて頂きました。
Sepsis Golden Hour 4 hour
The first World Sepsis Day will take place on September 13th. We anticipate that it will be supported by a fanfare of events around the world, with each of our member countries organizing events, securing media coverage, and engaging professional and public bodies together with health worker champions and people who have been personally affected by sepsis.
For the first time, we will have a clear focus on sepsis which extends beyond professional and academic needs. This will give the global sepsis community the identity it requires to create and maintain effective collaborations which will help not only to fuel the desire, but also to provide the means and infrastructure to make a difference with sepsis.
5つの世界的到達点(Global Goals)
1)敗血症の政策課題化
2)敗血症診療関係者の動員
3)敗血症診療ガイドライン実施のサポート
4)敗血症発症率と敗血症死亡率の低下
5)敗血症に対する十分な治療とリハビリテーション
2020年までの5つの目標 Key targets to be achieved by 2020
1)感染症予防により発症率を20%以上減少させる
2)早期発見と緊急治療により生存率を10%以上増加させる
3)一般市民および診療従事者への敗血症への注意喚起を徹底する
4)リハビリテーションサービスとの連動を充実させる
5)敗血症症例登録の国際化を推進する

Overview of Pyridine Nucleotides Review Series
Michinari Nakamura, Aruni Bhatnagar, and Junichi Sadoshima
Circulation Research. 2012;111:604-610
Regulation of Cell Survival and Death by Pyridine Nucleotides
Shin-ichi Oka, Chiao-Po Hsu, and Junichi Sadoshima
Circulation Research. 2012;111:611-627
Pyridine Nucleotide Regulation of Cardiac Intermediary Metabolism
John R. Ussher, Jagdip S. Jaswal, and Gary D. Lopaschuk
Circulation Research. 2012;111:628-641
Sirtuins and Pyridine Nucleotides
Maha Abdellatif
Circulation Research. 2012;111:642-656
Russel J. Reiter, Dun Xian Tan, Emilio Sanchez-Barcelo, Maria D. Mediavilla, Eloisa Gitto, Ahmet Korkmaz. J Exp Integr Med. 2011; 1(1): 13-22
In the past two decades, the results of a number of epidemiological studies have uncovered an association between excessive light exposure at night and the prevalence of cancer. Whereas the evidence supporting this link is strongest between nighttime light and female breast and male prostate cancer, the frequency of other tumor types may also be elevated. Individuals who have the highest reported increase in cancer are chronic night shift workers and flight attendants who routinely fly across numerous time zones.
There are at least two obvious physiological consequences of nighttime light exposure, i.e., a reduction in circulating melatonin levels and disruption of the circadian system (chronodisruption). Both these perturbations in experimental animals aggravate tumor growth. Melatonin has a long investigative history in terms of its ability to stymie the growth of many tumor types. Likewise, in the last decade chronodisruption has been unequivocally linked to a variety of abnormal metabolic conditions including excessive tumor growth.
This brief review summarizes the processes by which light after darkness onset impedes melatonin production and disturbs circadian rhythms. The survey also reviews the evidence associating the ostensible danger of excessive nighttime light pollution to cancer risk. If an elevated tumor frequency is definitively proven to be a consequence of light at night and/or chronodisruption, it seems likely that cancer will not be the exclusive pathophysiological change associated with the rampant light pollution characteristic of modern societies.
2. Beneficial effects of endogenous and exogenous melatonin on neural reconstruction and functional recovery in an animal model of spinal cord injury 2012; 52(1): 107.
The purpose of this study was to investigate the beneficial effects of endogenous and exogenous melatonin on functional recovery in an animal model of spinal cord injury (SCI). Eight-week-old male Sprague-Dawley (SD, 250–260 g) rats were used for contusion SCI surgery. All experimental groups were maintained under one of the following conditions: 12/12-hr light/dark (L/D) or 24:0-hr constant light (LL). Melatonin (10 mg/kg) was injected subcutaneously for 4 wk, twice daily (07:00, 19:00). Locomotor recovery, inducible nitric oxide synthase (iNOS), glial fibrillary acidic protein gene expression, and muscle atrophy-related genes, including muscle atrophy F-box (MAFbx) and muscle-specific ring-finger protein 1 (MuRF1) gene expression were evaluated. Furthermore, autophagic signaling such as Beclin-1 and LC3 protein expression was examined in the spinal cord and in skeletal muscle. The melatonin treatment resulted in increased hind-limb motor function and decreased iNOS mRNA expression in the L/D condition compared with the LL condition (P < 0.05), indicating that endogenous melatonin had neuroprotective effects. Furthermore, the MAFbx, MuRF1 mRNA level, and converted LC3 II protein expression were decreased in the melatonin-treated SCI groups under the LL (P < 0.05), possibly in response to the exogenous melatonin treatment. Therefore, it seems that both endogenous and exogenous melatonin contribute to neural recovery and to the prevention of skeletal muscle atrophy, promoting functional recovery after SCI. Finally, this study supports the benefit of endogenous melatonin and use of exogenous melatonin as a therapeutic intervention for SCI.
3. Glucose: A vital toxin and potential utility of melatonin in protecting against the diabetic state
Molecular and Cellular Endocrinology 2012; 349(2): 128.
The molecular mechanisms including elevated oxidative and nitrosative reactants, activation of pro-inflammatory transcription factors and subsequent inflammation appear as a unified pathway leading to metabolic deterioration resulting from hyperglycemia, dyslipidemia, and insulin resistance. Consistent evidence reveals that chronically-elevated blood glucose initiates a harmful series of processes in which toxic reactive species play crucial roles. As a consequence, the resulting nitro-oxidative stress harms virtually all biomolecules including lipids, proteins and DNA leading to severely compromised metabolic activity. Melatonin is a multifunctional indoleamine which counteracts several pathophysiologic steps and displays significant beneficial effects against hyperglycemia-induced cellular toxicity. Melatonin has the capability of scavenging both oxygen and nitrogen-based reactants and blocking transcriptional factors which induce pro-inflammatory cytokines. These functions contribute to melatonin’s antioxidative, anti-inflammatory and possibly epigenetic regulatory properties. Additionally, melatonin restores adipocyte glucose transporter-4 loss and eases the effects of insulin resistance associated with the type 2 diabetic state and may also assist in the regulation of body weight in these patients. Current knowledge suggests the clinical use of this non-toxic indoleamine in conjunction with other treatments for inhibition of the negative consequences of hyperglycemia for reducing insulin resistance and for regulating the diabetic state.
4. Plasma Melatonin and Urinary 6-Hydroxymelatonin Levels in Patients with Pulmonary Tuberculosis
Inflammation 2012
Tuberculosis (TB) is the second most frequent cause of death in the world, after AIDS. Delay in diagnosing TB is an important worldwide problem. It seriously threatens public health. Cell-mediated immune responses play an important role in the pathogenesis of TB infection. The course of Mycobacterium tuberculosis (MTb) infection is regulated by two distinct T cell cytokine patterns. Melatonin is a biomolecule (mainly secreted by the pineal gland) with free radical scavenging, antioxidant and immunoregulatory properties. Melatonin has both its direct and indirect immunomodulatory effects on the immune system. In this study, we measured plasma melatonin and urine 6-hydroxy melatonin sulphate (6-HMS) concentrations in patients with newly diagnosed TB for the purpose of investigating whether there was a relationship between their levels and MTb infection. Thirty-one newly diagnosed patients presenting with active TB and 31 healthy subjects as the control group were included in this study. Blood and 24-h urine samples were collected from all individuals. Plasma melatonin levels and urine 6-HMS were measured. Our results show that in patients with TB, mean melatonin and 6-HMS concentrations were significantly lower than in the control subjects (p = 0.037, p < 0.001, respectively). We believe that the treatment of TB patients with melatonin might result in a wide range of health benefits including improved quality of life and reduced severity of infection in these patients. Supplementation with melatonin may be considered as an adjunctive therapy to classic treatment of pulmonary TB, especially during the acute phase of infection.
5. Beneficial actions of melatonin in the management of viral infections: a new use for this “molecular handyman”?
Rev. Med. Virol. 2012
Melatonin (N-acetyl-5-methoxytryptamine) is a multifunctional signaling molecule that has a variety of important functions. Numerous clinical trials have examined the therapeutic usefulness of melatonin in different fields of medicine. Clinical trials have shown that melatonin is efficient in preventing cell damage under acute (sepsis, asphyxia in newborns) and chronic states (metabolic and neurodegenerative diseases, cancer, inflammation, aging). The beneficial effects of melatonin can be explained by its properties as a potent antioxidant and antioxidant enzyme inducer, a regulator of apoptosis and a stimulator of immune functions. These effects support the use of melatonin in viral infections, which are often associated with inflammatory injury and increases in oxidative stress. In fact, melatonin has been used recently to treat several viral infections, which are summarized in this review. The role of melatonin in infections is also discussed herein. Copyright © 2012 John Wiley & Sons, Ltd.
6. Gene regulation by melatonin linked to epigenetic phenomena
Gene 2012:503;1-11
Many exogenous (e.g., toxins, chemicals, ultraviolet, cigarette smoke) and endogenous (e.g., hyperglycemia, dyslipidemia, cytokines, chemokines) agents disrupt the intracellular environment and result in a massive production of reactive oxygen species (ROS) and reactive nitrogen species (RNS). The molecular damage that ROS/RNS induce is referred to as nitrooxidative stress. The cellular consequences of nitrooxidative stress include lipid peroxidation, protein oxidation and DNA damage. Additionally, ROS and RNS deplete cellular defenses and initiate inflammation. It is widely accepted that nitrooxidative stress and inflammation play important roles in the pathogenesis of a variety of human diseases and sequelae. Several processes are crucial to overcome the damaging cellular events caused by nitrooxidative stress, e.g., scavenging both ROS and RNS, induction of defense mechanisms and alleviating/suppressing inflammation are essential. Both endogenous and pharmacological concentrations of melatonin have long been known to play role in the direct scavenging of ROS and RNS as well as inducing antioxidant defense mechanisms and ameliorating inflammation. The current review summarizes research related to two major transcription factors that participate in these processes and summarizes how melatonin regulates antioxidant and pro-inflammatory genes via epigenetic on/off mechanisms.
<font color="red">7. Melatonin in bacterial and viral infections with focus on sepsis: a review.
Srinivasan V, Mohamed M, Kato H.
Recent Pat Endocr Metab Immune Drug Discov. 2012 Jan;6(1):30-9. Review.
この総説は読まれてみて下さい。敗血症におけるメラトニン研究は,現在このレベルで留まっています。
Melatonin is a versatile molecule, synthesized not only by the pineal gland, but also in small amounts by many other organs like retina, gastrointestinal tract, thymus, bone marrow, lymphocytes etc. It plays an important role in various functions of the body like sleep and circadian rhythm regulation, immunoregulatory mechanism, free radical scavenger, antioxidant functions, oncostatic actions, control of reproductive functions, regulation of mood etc. Melatonin has also been found to be effective in combating various bacterial and viral infections. Its administration has been shown to be effective in controlling chlamydial infections, infections induced by Mycobacterium tuberculosis, and also in many viral infections. Molecular mechanisms of anti microbial actions of melatonin have suggested to be due to effects on free radical formation, direct regulation of duplication of bacteria, depletion of intracellular substrates like iron etc. Besides, it is effective in sepsis as demonstrated in various animal models of septic shock. Melatonin's protective action against sepsis is suggested to be due to its antioxidant, immunomodulating and inhibitory actions against the production and activation of pro-inflammatory mediators. Use of melatonin has been beneficial in treating premature infants suffering from severe respiratory distress syndrome and septic shock. It has a potential therapeutic value in treating septic shock and associated multi organ failure in critically ill patients in addition to its antimicrobial and antiviral actions. The patents related to melatonin's use for treatment of bacterial infections and its use in clinical disorders are included.
8. Melatonin in septic shock: some recent concepts.
Srinivasan V, Pandi-Perumal SR, Spence DW, Kato H, Cardinali DP.
J Crit Care. 2010 Dec;25(4):656.e1-6.
Melatonin is a versatile molecule, synthesized not only in the pineal gland, but also in many other organs. Melatonin plays an important physiologic role in sleep and circadian rhythm regulation, immunoregulation, antioxidant and mitochondrial-protective functions, reproductive control, and regulation of mood. Melatonin has also been reported as effective in combating various bacterial and viral infections. Melatonin is an effective anti-inflammatory agent in various animal models of inflammation and sepsis, and its anti-inflammatory action has been attributed to inhibition of nitric oxide synthase with consequent reduction of peroxynitrite formation, to the stimulation of various antioxidant enzymes thus contributing to enhance the antioxidant defense, and to protective effects on mitochondrial function and in preventing apoptosis. In a number of animal models of septic shock, as well as in patients with septic disease, melatonin reportedly exerts beneficial effects to arrest cellular damage and multiorgan failure. The significance of these actions in septic shock and its potential usefulness in the treatment of multiorgan failure are discussed.
The new intensivist
James Goodwin, Simon Baudouin, Julian Bion
日本集中治療医学会では,現在,集中治療専門医制度を見直し,専門医取得のための認定プログラムを作成しています。日本専門医制評価・認定機構の第1類(I.基本領域専門医学会)の専門医資格として救急科専門医などは,サブスペシャリティとして集中治療専門医資格を取るとよいです。本邦には300名程度しか,実働している集中治療専門医はいないと言われていますが,これからの集中治療専門医により集中治療医学のレベルを高め,優秀な診療と診療成績を提供することが大切です。いずれにしても,急性期医学と急性期診療を専門診療科として牽引するなかで,このような英国のnew intensivistの新しい概念についても御一考ください。 (コメント 松田直之)
Training in intensive care medicine in the United Kingdom is about to undergo major changes. From August 2012 trainees will be able to enter a standalone certificate of completion of training (CCT) programme in intensive care medicine, after competitive entry at specialty training year 3 (ST3) level. On their successful completion, these programmes will lead to the award of a CCT in intensive care medicine.
The approval by the General Medical Council (GMC) of a new standalone CCT programme marks a “coming of age” for the specialty. Intensive care medicine arose from the need to provide treatment for patients with severe physiological disturbances within fixed, specialist clinical areas. As the specialty developed and the number of dedicated beds grew, it became clear that the broad remit of intensive care medicine required a dedicated training programme. In the UK this originally took the form of a so called joint CCT programme, whereby trainees entering intensive care medicine training had to be already enrolled in a complementary specialty CCT programme, usually anaesthesia, emergency medicine, or a medical specialty. On entry to the joint CCT programme, trainees received training in intensive care medicine and in “complementary” skills (such as anaesthesia for physician entrants).
The new intensive care medicine CCT programme is a logical development of the previous joint CCT programme. It completely fulfils the GMC’s requirements for a specialty programme in that it defines the totality of training and competencies required, with a detailed, competency based syllabus and assessment system.
Entry and progression through intensive care medicine training
Entry to the intensive care medicine CCT programme in August 2012 will be at ST3 level. Entry will be competitive, with national selection and ranking in England and Wales using identical processes to other current CCT programmes. Entry to higher specialist training in intensive care medicine differs from most other CCTs in that it deliberately does not have one single core programme. The new Faculty of Intensive Care Medicine, supported by its constituent royal colleges and the GMC, wanted to see the established multidisciplinary approach to intensive care medicine training continue. Trainees applying for higher specialist training in intensive care medicine can enter by any one of three separate routes: core anaesthetic training, core medical training, or any of the acute common care stem strands. Successful candidates will then enter intensive care medicine at ST3 level with different training experiences and competencies.
For example, core medical trainees will have few or no skills in anaesthesia, and core anaesthetic trainees will have little experience in the assessment and management of severely ill patients in medical admission wards. The first two years of higher training in intensive care medicine (ST3 and ST4) were designed to allow an individualised programme of training so that all trainees would achieve the same level of competency by the end of ST4. The first four years of intensive care medicine training (CT1 to ST4) are designated stage 1.
Stage 2 training occurs in ST5 and ST6, and the exact sequence of attachments will vary from scheme to scheme. During these years trainees will consolidate their general training in intensive care medicine as well as develop specialist skills. Competencies will be gained in the management of critically ill neurosurgical and cardiothoracic patients. Experience in the management of severely ill children will also be gained; however, the intensive care medicine CCT programme is not aimed at providing advanced training in paediatric intensive care medicine.
Stage 2 training also allows a period of acquisition of special skills. This develops the multidisciplinary philosophy of intensive care medicine training by allowing trainees to choose from various modules. These are currently being developed but will include training in advanced imaging techniques, research methodology, and audit and quality improvement techniques. Some trainees may also choose to enhance their specialist skills with further training in cardiothoracic or neurosurgical intensive care medicine.
Stage 3 training (ST7) is designed to allow trainees to enhance further their competencies in intensive care medicine, with an emphasis on organisational, management, and quality aspects of the specialty.
Assessments and examinations
The intensive care medicine CCT assessment system will be familiar to all foundation trainees. It consists of well validated workplace based assessment tools, which are used to determine progress against the training syllabus. There will also be a higher fellow of the Faculty of Intensive Care Medicine (FFICM) examination, which will use a number of assessment methods, including multiple choice questions, structured vivas, and objective structured clinical exam (OSCE)-style skill stations. Passing the FFICM will be a requirement for entry to stage 3 training.
Syllabus
Intensive care medicine is a broad discipline. On any given day an intensive care practitioner may be asked to assess, diagnose, and treat critically ill patients with common and more esoteric problems. The formal syllabus reflects this need for broad based knowledge and training. It has been built around the European Society of Intensive Care Medicine’s CoBaTrICE competency based training programme (www.cobatrice.org), which used consensus methods and extensive public consultation to develop and define core knowledge, attitudes, and skills in intensive care medicine. The UK programme and its European progenitor remain dynamic works in progress, which will evolve to reflect changes in intensive care practice as new evidence emerges. The new UK curriculum is available at www.ficm.ac.uk/icmcctcurriculum.ashx.
Dual CCTs
While some trainees may want to follow a career in intensive care medicine only, many are likely to want to pair this with a second CCT in anaesthesia, emergency medicine, or one of the medical specialties (respiratory medicine, for example). In 2012, trainees in existing CCT programmes will still be able to apply for the old joint CCT programme. In 2013 this will be replaced by the new dual CCT programme. Trainees who wish to train in both intensive care medicine and a partner specialty will be able to do this by a stepped entry method.
They will initially need to compete for their first CCT post and then within 18 months to compete for their second CCT post. For example, a trainee who enters an intensive care medicine CCT programme in August 2012 will have until February 2014 to enter a partner CCT programme. Alternatively, a trainee in a partner CCT programme from August 2012 can, within 18 months, apply for an intensive care medicine CCT programme.
The total duration of training needed to achieve dual CCT accreditation will, of necessity, be longer than that for a single CCT. However, the Faculty of Intensive Care Medicine, with the GMC, is identifying those competencies that can be acquired in either part of a dual programme. It is therefore likely that the total duration of dual training will not exceed 8.5 years in most cases.
A career in intensive care medicine?
No single attribute can define a successful practitioner in intensive care medicine, but it is likely that most consultants will have a preference for being a “complete physician” in the sense that they have broad knowledge of many diseases and treatments; possess advanced technical and non-technical skills in physiological and emotional support of patients and their families; have the capacity to integrate care across disciplines, locations, and time; are simultaneously team players and team leaders; and teach and inspire others by example. More specifically:
They are interested in acute physiology and the way in which human physiology can be manipulated to improve outcomes in severely ill patients.
They can rapidly assimilate and integrate large amounts of complex data (including those from physical examination and history taking).
They can make rapid and decisive action plans in the face of often considerable clinical uncertainty.
They are able to both lead and contribute to truly multidisciplinary clinical teams.
They are good negotiators for their patients. Intensive care medicine consultants will often have a role as care coordinator, acting as an intermediary between clinical teams.
They are comfortable with and skilled at performing practical procedures.
They can “multitask” in situations that are often pressured in terms of both time and work intensity.
They accept that intensive care medicine work is unpredictable and often occurs outside normal hours.
However, a career in intensive care medicine is not just about immediate care. A good intensivist is also interested in longer term problems, and many intensivists now follow up their patients after discharge from the intensive care unit. Effective practitioners are also good managers and are interested in improving the quality of their service. Intensive care medicine was one of the first specialties to organise comprehensive national units, and this work continues to inform the design and delivery of services.
Job prospects
These are good. In the first year it is likely that more than 60 additional intensive care medicine CCT posts will be released, bringing the total number to more than 200. This will probably increase in future years to reflect the need for more consultants in intensive care medicine.
Summary of the new CCT programme in intensive care medicine
Competitive entry to a new standalone intensive care medicine CCT programme is possible from August 2012.
Initial entry will be at ST3 level.
Core trainees from anaesthesia, emergency medicine, or medicine who have obtained their respective exams for progression to higher training can apply for the programme.
The indicative duration of the programme is seven years, divided into three stages of training: CT1 to ST4; ST5 and ST6; and ST7.
Current CCT trainees in anaesthesia, emergency medicine, medicine, and surgery can apply to the old joint CCT programme until August 2013.
From August 2013 trainees can competitively apply to a second, complementary CCT programme to acquire dual intensive care medicine and complementary specialty CCTs.