High-Flow Oxygen through Nasal Cannula in Acute Hypoxemic Respiratory Failure.
FLORALI Study Group and the REVA Network.
Frat JP, Thille AW, Mercat A, Girault C, Ragot S, Perbet S, Prat G, Boulain T, Morawiec E, Cottereau A, Devaquet J, Nseir S, Razazi K, Mira JP, Argaud L, Chakarian JC, Ricard JD, Wittebole X, Chevalier S, Herbland A, Fartoukh M, Constantin JM, Tonnelier JM, Pierrot M, Mathonnet A, Béduneau G, Delétage-Métreau C, Richard JC, Brochard L, Robert R; FLORALI Study Group and the REVA Network.
N Engl J Med. 2015 Jun 4;372(23):2185-2196.
Background Whether noninvasive ventilation should be administered in patients with acute hypoxemic respiratory failure is debated. Therapy with high-flow oxygen through a nasal cannula may offer an alternative in patients with hypoxemia.
Methods We performed a multicenter, open-label trial in which we randomly assigned patients without hypercapnia who had acute hypoxemic respiratory failure and a ratio of the partial pressure of arterial oxygen to the fraction of inspired oxygen of 300 mm Hg or less to high-flow oxygen therapy, standard oxygen therapy delivered through a face mask, or noninvasive positive-pressure ventilation. The primary outcome was the proportion of patients intubated at day 28; secondary outcomes included all-cause mortality in the intensive care unit and at 90 days and the number of ventilator-free days at day 28.
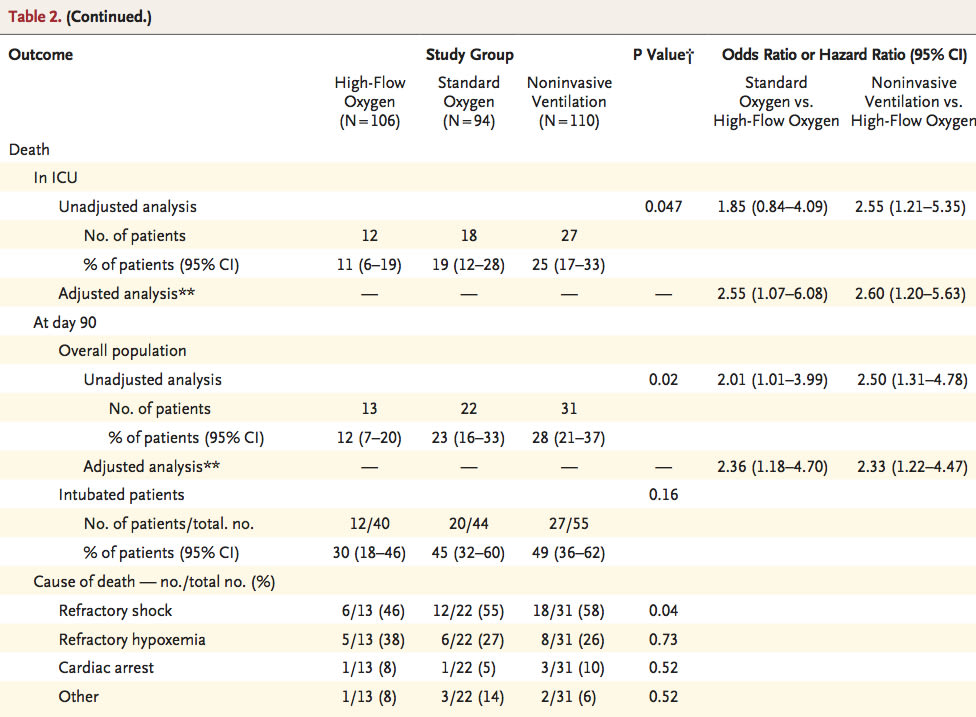
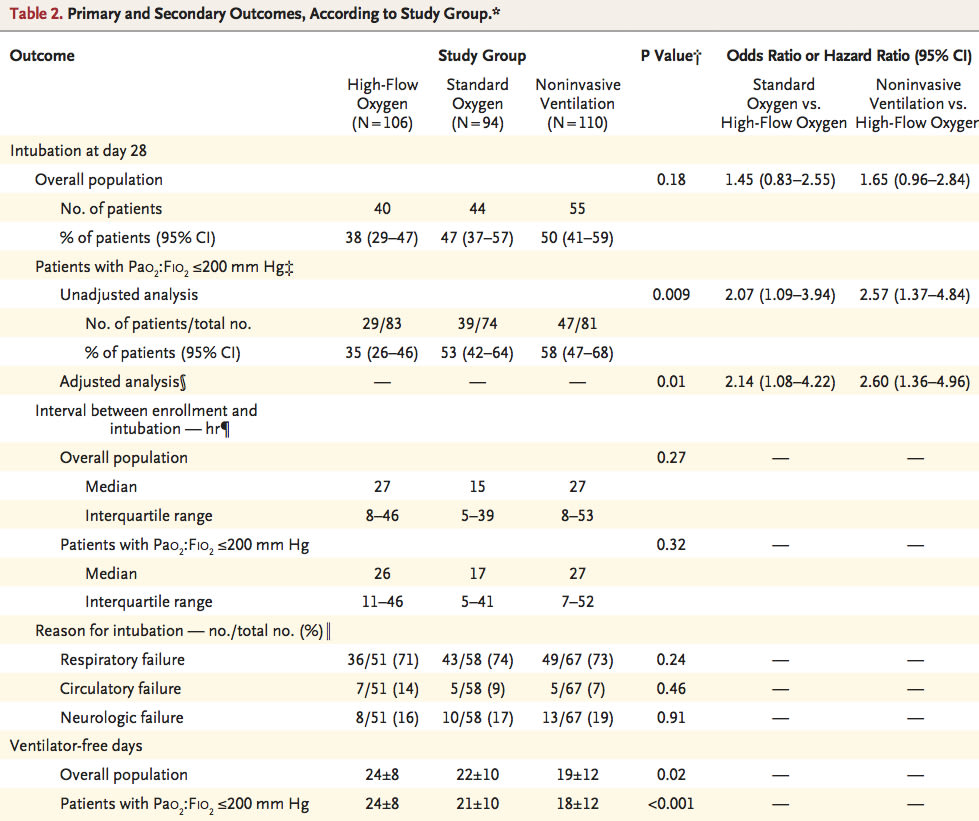
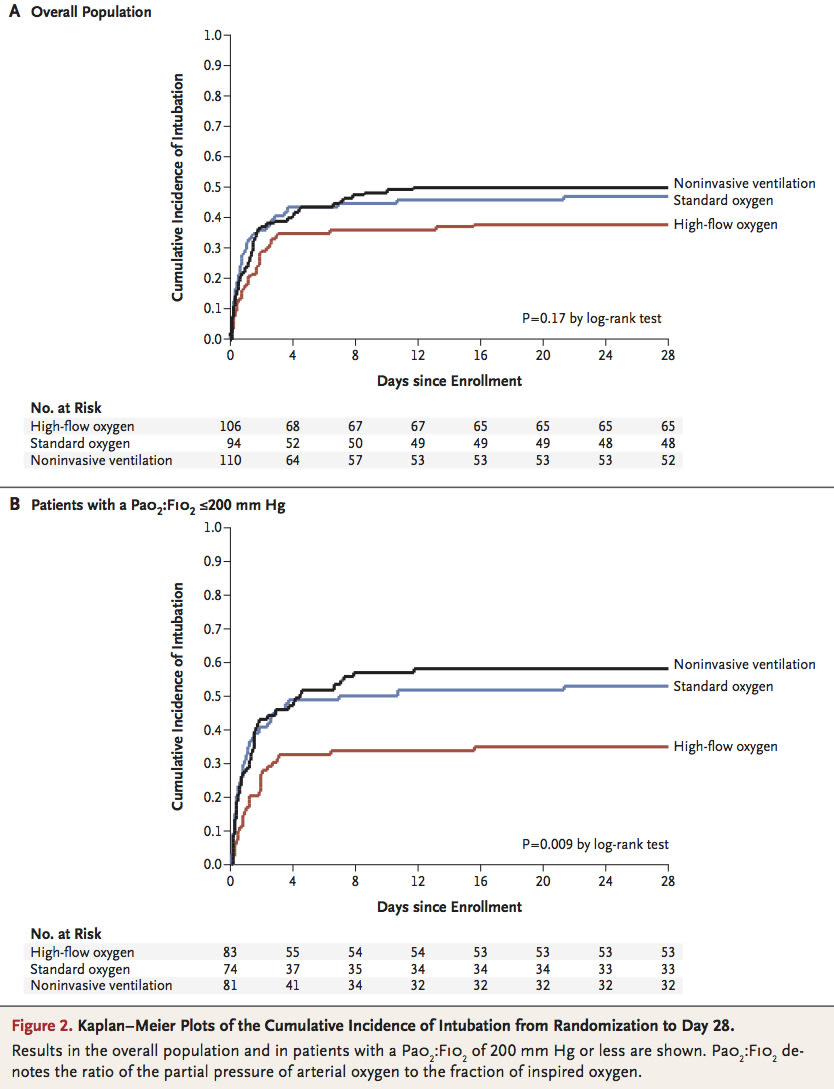
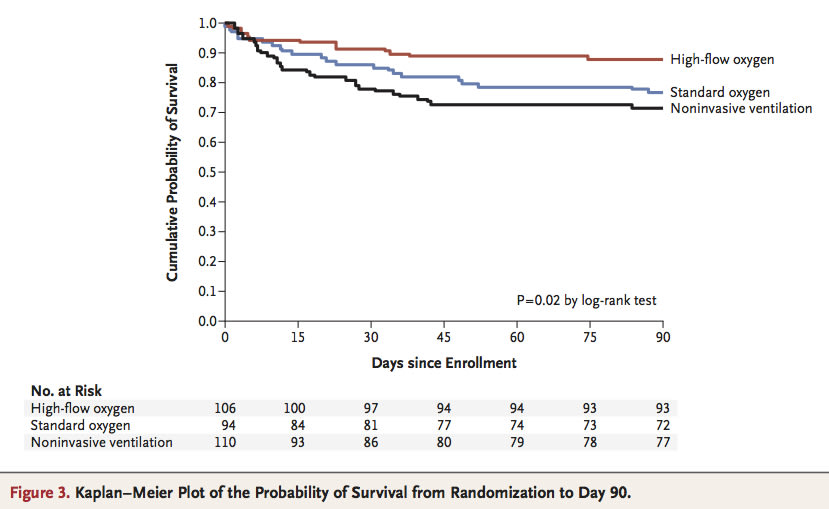
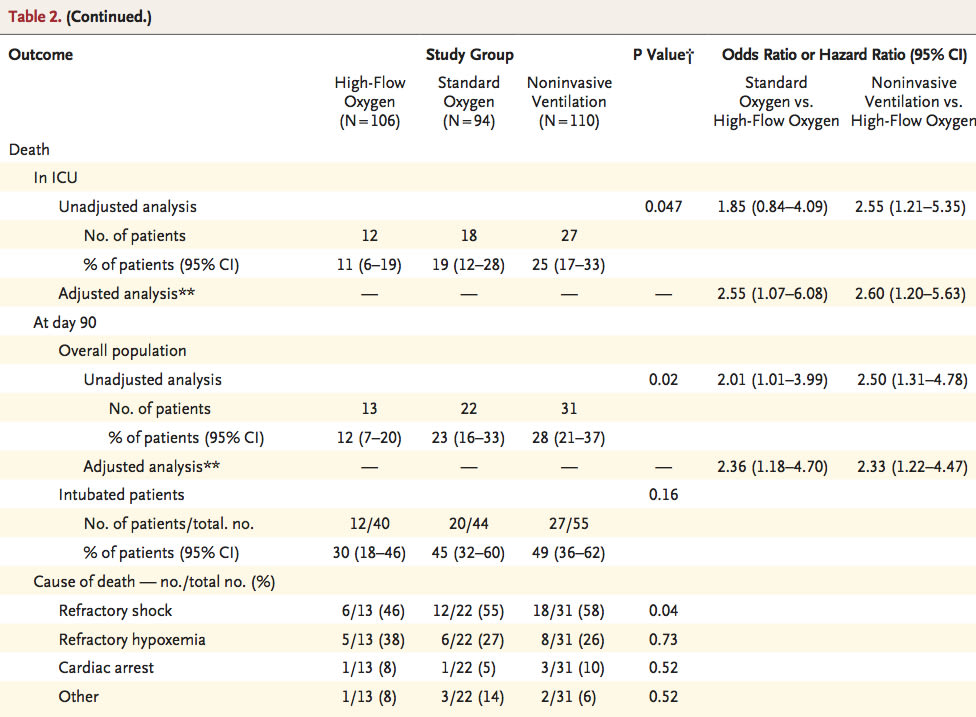
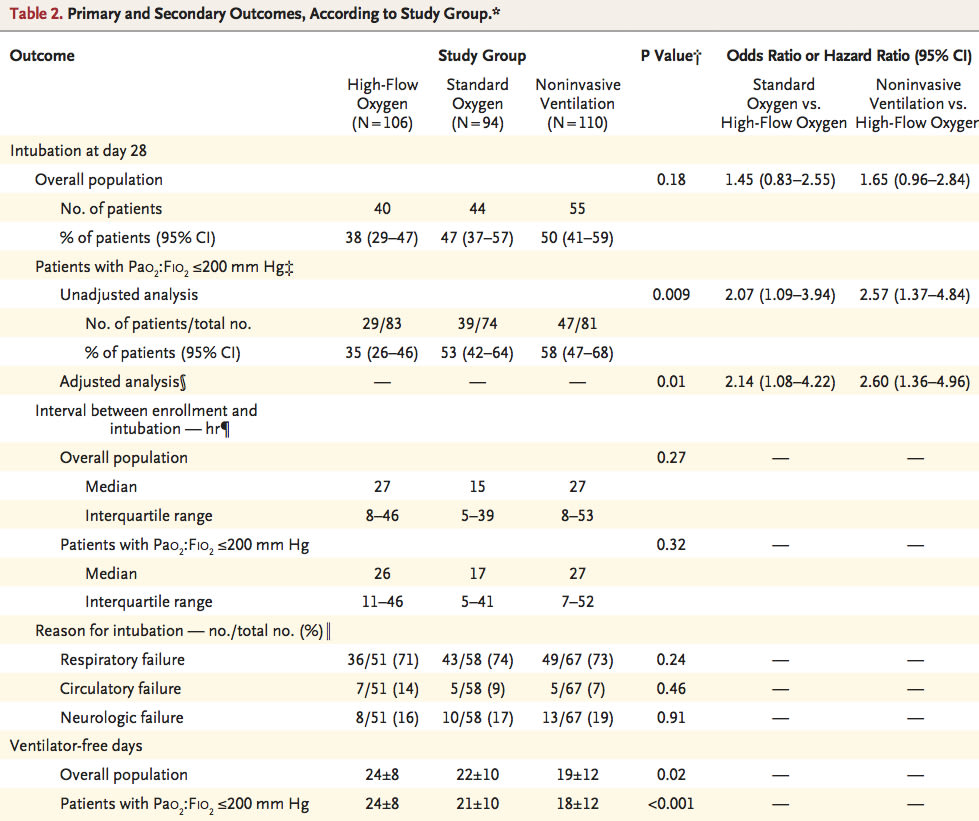
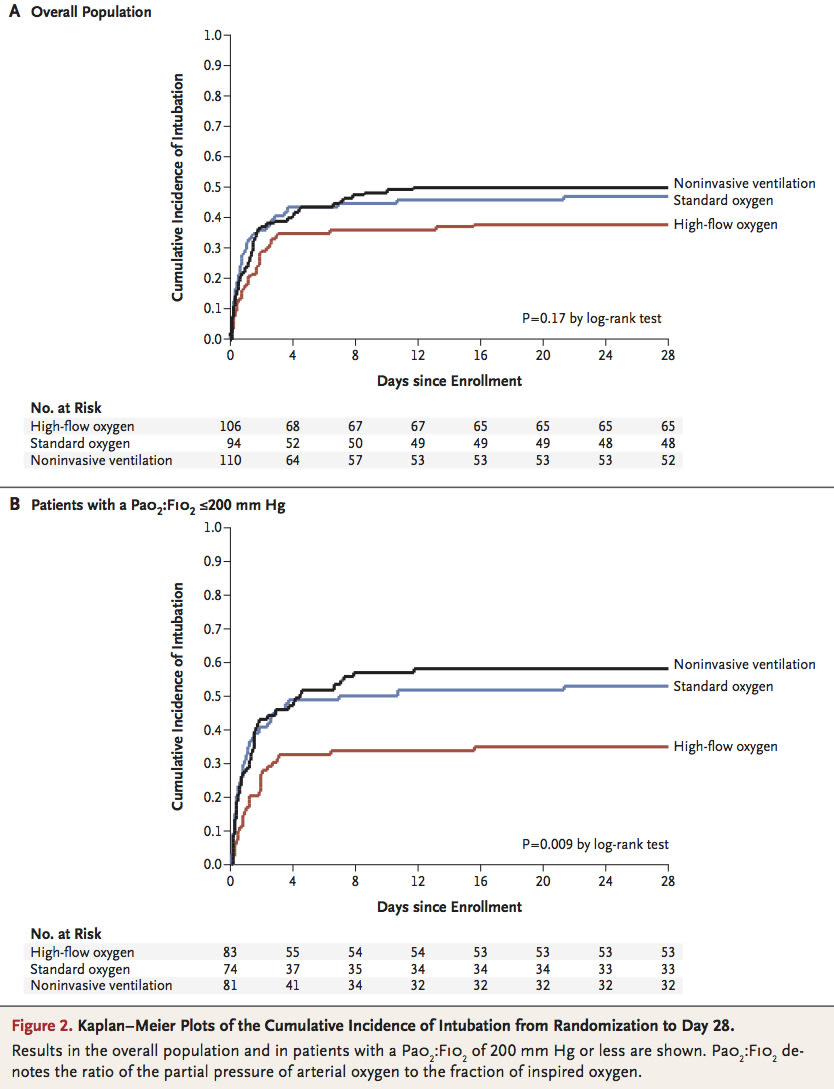
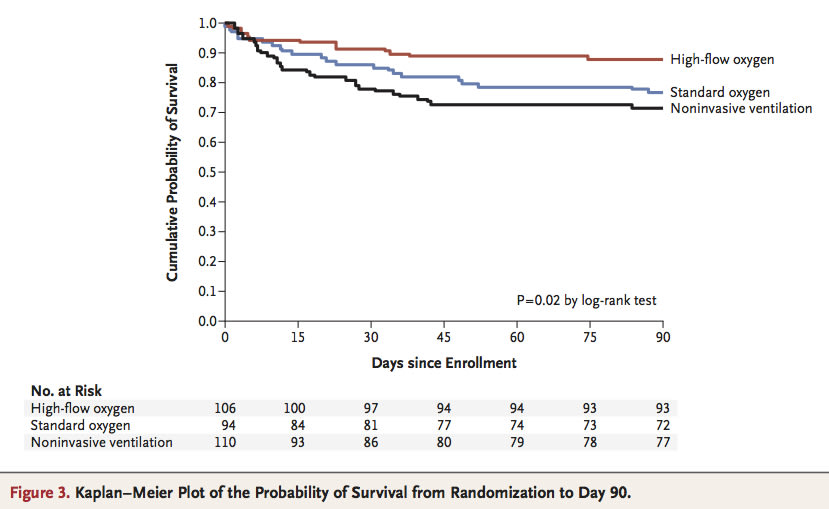
Results A total of 310 patients were included in the analyses. The intubation rate (primary outcome) was 38% (40 of 106 patients) in the high-flow-oxygen group, 47% (44 of 94) in the standard group, and 50% (55 of 110) in the noninvasive-ventilation group (P=0.18 for all comparisons). The number of ventilator-free days at day 28 was significantly higher in the high-flow-oxygen group (24±8 days, vs. 22±10 in the standard-oxygen group and 19±12 in the noninvasive-ventilation group; P=0.02 for all comparisons). The hazard ratio for death at 90 days was 2.01 (95% confidence interval [CI], 1.01 to 3.99) with standard oxygen versus high-flow oxygen (P=0.046) and 2.50 (95% CI, 1.31 to 4.78) with noninvasive ventilation versus high-flow oxygen (P=0.006).
Conclusions In patients with nonhypercapnic acute hypoxemic respiratory failure, treatment with high-flow oxygen, standard oxygen, or noninvasive ventilation did not result in significantly different intubation rates. There was a significant difference in favor of high-flow oxygen in 90-day mortality. (Funded by the Programme Hospitalier de Recherche Clinique Interrégional 2010 of the French Ministry of Health; FLORALI ClinicalTrials.gov number, NCT01320384 .).
<松田直之 コメント> MEIDAI救急・集中治療は2012年よりHFNCを導入し,全身性炎症の改善に末梢気道開放ブランチを設定してきました。我々のデータと同様に,本論文でもHFNCによるopen lungにより,生命予後が有意に改善しています。気管挿管リスクをNPPVは低下させていないのですが,P/F比≦200 mmHgがHFNCでは少ないです。本論文は,2011年2月から2013年4月までにフランスとベルギーの23のICUにおける酸素化の臨床研究ですが,このREVA(Reseau Europeen de Recherche en Ventilation Artificielle)Networkの治療成績も良くなってきています。
※ FLORALI trial:Non- invasive Ventilation and High Flow Nasal Oxygen Therapy in Resuscitation of Pa- tients with Acute Lung Injury trial

母体数を維持する上で,40.4%(212/525)脱落率は高いように思います。
参考文献
1. Blodgett AN. The continuous inhalation of oxygen in cases of pneumonia otherwise fatal, and in other diseases. Boston Med J 1890;123:481-5.
2. Brochard L, Mancebo J, Wysocki M, et al. Noninvasive venti- lation for acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med 1995;333:817-22.
3. Keenan SP, Sinuff T, Cook DJ, Hill NS. Which patients with acute exacerbation of chronic obstructive pulmonary disease benefit from noninvasive positive-pressure ventilation? A sys- tematic review of the literature. Ann Intern Med 2003;138:861- 70.
4. Masip J, Roque M, Sánchez B, Fernández R, Subirana M, Expósito JA. Noninvasive ventilation in acute cardiogenic pul- monary edema: systematic review and meta-analysis. JAMA 2005;294:3124-30.
5. Ward JJ. High-flow oxygen administration by nasal cannula for adult and perinatal patients. Respir Care 2013;58:98-122.
6. Patel A, Nouraei SAR. Transnasal humidified rapid-insuffla- tion ventilatory exchange (THRIVE): a physiological method of increasing apnoea time in patients with difficult airways. An- aesthesia 2015;70:323-9.
7. Maggiore SM, Idone FA, Vaschetto R, et al. Nasal high-flow oxygenation, comfort, and clinical outcome. Am J Respir Crit Care Med 2014;190:282-8.
8. Frat J-P, Thille AW, Mercat A, et al. High-flow versus Venturi mask oxygen therapy after extubation: effects on oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med 2015;372:2185-96.
9. Nuckton TJ, Alonso JA, Kallet RH, et al. Pulmonary dead- space fraction as a risk factor for death in the acute respiratory distress syndrome. N Engl J Med 2002;346:1281-6.
10. The Acute Respiratory Distress Syndrome Network. Ventila- tion with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 2000;342:1301-8.
FLORALI Study Group and the REVA Network.
Frat JP, Thille AW, Mercat A, Girault C, Ragot S, Perbet S, Prat G, Boulain T, Morawiec E, Cottereau A, Devaquet J, Nseir S, Razazi K, Mira JP, Argaud L, Chakarian JC, Ricard JD, Wittebole X, Chevalier S, Herbland A, Fartoukh M, Constantin JM, Tonnelier JM, Pierrot M, Mathonnet A, Béduneau G, Delétage-Métreau C, Richard JC, Brochard L, Robert R; FLORALI Study Group and the REVA Network.
N Engl J Med. 2015 Jun 4;372(23):2185-2196.
Background Whether noninvasive ventilation should be administered in patients with acute hypoxemic respiratory failure is debated. Therapy with high-flow oxygen through a nasal cannula may offer an alternative in patients with hypoxemia.
Methods We performed a multicenter, open-label trial in which we randomly assigned patients without hypercapnia who had acute hypoxemic respiratory failure and a ratio of the partial pressure of arterial oxygen to the fraction of inspired oxygen of 300 mm Hg or less to high-flow oxygen therapy, standard oxygen therapy delivered through a face mask, or noninvasive positive-pressure ventilation. The primary outcome was the proportion of patients intubated at day 28; secondary outcomes included all-cause mortality in the intensive care unit and at 90 days and the number of ventilator-free days at day 28.
Results A total of 310 patients were included in the analyses. The intubation rate (primary outcome) was 38% (40 of 106 patients) in the high-flow-oxygen group, 47% (44 of 94) in the standard group, and 50% (55 of 110) in the noninvasive-ventilation group (P=0.18 for all comparisons). The number of ventilator-free days at day 28 was significantly higher in the high-flow-oxygen group (24±8 days, vs. 22±10 in the standard-oxygen group and 19±12 in the noninvasive-ventilation group; P=0.02 for all comparisons). The hazard ratio for death at 90 days was 2.01 (95% confidence interval [CI], 1.01 to 3.99) with standard oxygen versus high-flow oxygen (P=0.046) and 2.50 (95% CI, 1.31 to 4.78) with noninvasive ventilation versus high-flow oxygen (P=0.006).
Conclusions In patients with nonhypercapnic acute hypoxemic respiratory failure, treatment with high-flow oxygen, standard oxygen, or noninvasive ventilation did not result in significantly different intubation rates. There was a significant difference in favor of high-flow oxygen in 90-day mortality. (Funded by the Programme Hospitalier de Recherche Clinique Interrégional 2010 of the French Ministry of Health; FLORALI ClinicalTrials.gov number, NCT01320384 .).
<松田直之 コメント> MEIDAI救急・集中治療は2012年よりHFNCを導入し,全身性炎症の改善に末梢気道開放ブランチを設定してきました。我々のデータと同様に,本論文でもHFNCによるopen lungにより,生命予後が有意に改善しています。気管挿管リスクをNPPVは低下させていないのですが,P/F比≦200 mmHgがHFNCでは少ないです。本論文は,2011年2月から2013年4月までにフランスとベルギーの23のICUにおける酸素化の臨床研究ですが,このREVA(Reseau Europeen de Recherche en Ventilation Artificielle)Networkの治療成績も良くなってきています。
※ FLORALI trial:Non- invasive Ventilation and High Flow Nasal Oxygen Therapy in Resuscitation of Pa- tients with Acute Lung Injury trial

母体数を維持する上で,40.4%(212/525)脱落率は高いように思います。
参考文献
1. Blodgett AN. The continuous inhalation of oxygen in cases of pneumonia otherwise fatal, and in other diseases. Boston Med J 1890;123:481-5.
2. Brochard L, Mancebo J, Wysocki M, et al. Noninvasive venti- lation for acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med 1995;333:817-22.
3. Keenan SP, Sinuff T, Cook DJ, Hill NS. Which patients with acute exacerbation of chronic obstructive pulmonary disease benefit from noninvasive positive-pressure ventilation? A sys- tematic review of the literature. Ann Intern Med 2003;138:861- 70.
4. Masip J, Roque M, Sánchez B, Fernández R, Subirana M, Expósito JA. Noninvasive ventilation in acute cardiogenic pul- monary edema: systematic review and meta-analysis. JAMA 2005;294:3124-30.
5. Ward JJ. High-flow oxygen administration by nasal cannula for adult and perinatal patients. Respir Care 2013;58:98-122.
6. Patel A, Nouraei SAR. Transnasal humidified rapid-insuffla- tion ventilatory exchange (THRIVE): a physiological method of increasing apnoea time in patients with difficult airways. An- aesthesia 2015;70:323-9.
7. Maggiore SM, Idone FA, Vaschetto R, et al. Nasal high-flow oxygenation, comfort, and clinical outcome. Am J Respir Crit Care Med 2014;190:282-8.
8. Frat J-P, Thille AW, Mercat A, et al. High-flow versus Venturi mask oxygen therapy after extubation: effects on oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med 2015;372:2185-96.
9. Nuckton TJ, Alonso JA, Kallet RH, et al. Pulmonary dead- space fraction as a risk factor for death in the acute respiratory distress syndrome. N Engl J Med 2002;346:1281-6.
10. The Acute Respiratory Distress Syndrome Network. Ventila- tion with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 2000;342:1301-8.