The diagnostic and prognostic significance of monitoring blood levels of immature neutrophils in patients with systemic inflammation.
Abstract
INTRODUCTION:
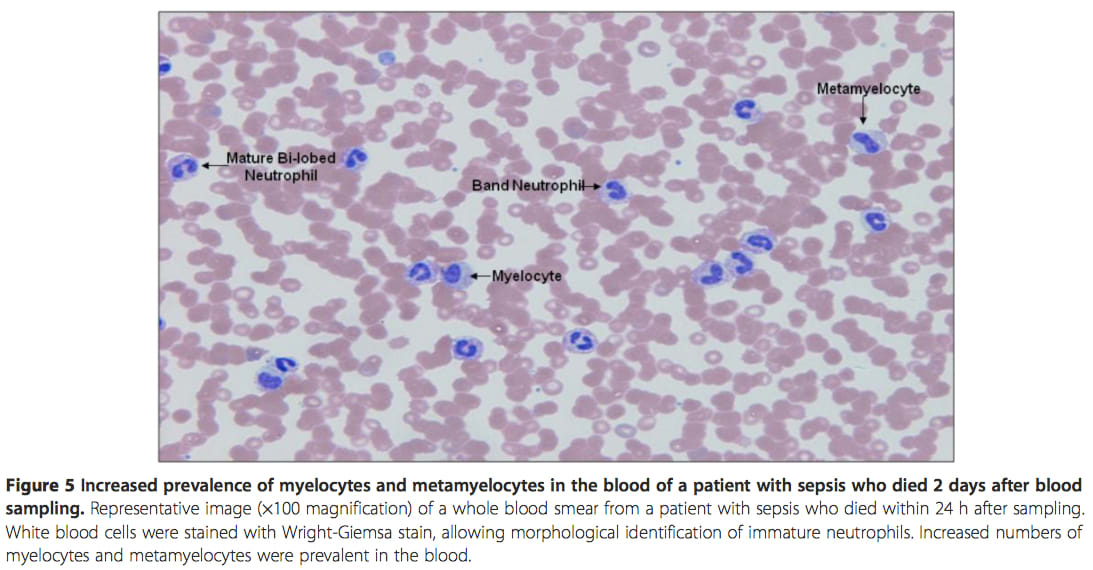
In this cohort study, we investigated whether monitoring blood levels of immature neutrophils (myelocytes, metamyelocytes and band cells) differentiated patients with sepsis from those with the non-infectious (N-I) systemic inflammatory response syndrome (SIRS). We also ascertained if the appearance of circulating immature neutrophils was related to adverse outcome.
METHODS:
Blood samples were routinely taken from 136 critically ill patients within 48 hours of ICU entry and from 20 healthy control subjects. Clinical and laboratory staff were blinded to each other's results, and patients were retrospectively characterised into those with SIRS (n = 122) and those without SIRS (n = 14). The patients with SIRS were further subdivided into categories of definite sepsis (n = 51), possible sepsis (n = 32) and N-I SIRS (n = 39). Two established criteria were used for monitoring immature white blood cells (WBCs): one where band cells >10% WBCs and the other where >10% of all forms of immature neutrophils were included but with a normal WBC count. Immature neutrophils in blood smears were identified according to nuclear morphology and cytoplasmic staining.
RESULTS:
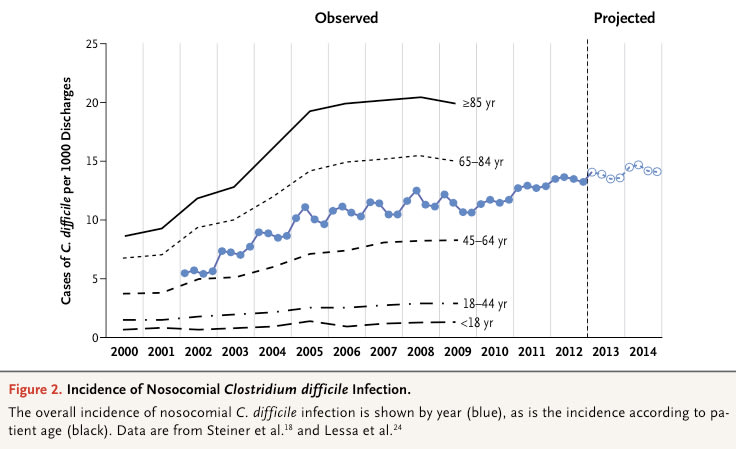
With the first criterion, band cells were present in most patients with SIRS (mean = 66%) when compared with no SIRS (mean = 29%; P
CONCLUSIONS:
Raised blood levels of band cells have diagnostic significance for sepsis, provided that measurements are not confined to patients with normal WBC counts, whereas an increased prevalence of myelocytes and metamyelocytes may have prognostic application.

Innate immune functions of immature neutrophils in patients with sepsis and severe systemic inflammatory response syndrome.
Abstract
OBJECTIVE:
A hallmark of sepsis and severe systemic inflammatory response syndrome (SIRS) is the massive recruitment of immature neutrophils from the bone marrow into the circulation (left shift, band forms). Their capacity to participate in innate defense against bacteria is ill defined. We aimed at comparing various innate immune functions of mature vs. immature neutrophils circulating during sepsis and SIRS.
DESIGN:
Prospective, observational cohort study.
SETTING:Tertiary level ICU and associated research laboratory.
PATIENTS:
Thirty-three ICU patients with sepsis; 12 ICUs with SIRS; 32 healthy volunteers.
INTERVENTIONS:
Twenty milliliters of whole heparinized blood was used for in vitro studies including neutrophil viability and apoptosis, surface expression of CD16, Toll-like receptors () 4 and TLR2, CD14, MD-2, HLA-DP,-DQ and -DR, and CXCR2, chemotaxis, phagocytosis, bacterial killing, and tumor necrosis factor-α/interleukin-10 baseline intracellular cytokine levels.
MEASUREMENTS AND MAIN RESULTS:
Immature neutrophils were capable of mediating important innate immune functions such as bacterial phagocytosis and killing via the production of reactive oxygen species, although less efficiently than mature neutrophils. Immature neutrophils had a longer life span and resistance to spontaneous apoptosis, and could mature ex vivo. They expressed lower levels of receptors for bacterial molecules such as CD14 and MD-2 and migrated less efficiently than mature granulocytes. Immature neutrophils had higher basal intracellular tumor necrosis factor-α/interleukin-10 ratio than that of mature neutrophils, suggesting a proinflammatory phenotype. No significant differences were observed between immature neutrophils isolated from patients with sepsis and those from patients with severe SIRS.
CONCLUSIONS:
Despite their "immaturity", band forms are capable of mediating crucial innate immune functions during severe infections and sepsis. Their fate and capacity to mature in vivo remain to be determined.