Comparison of Blood Pressures obtained with the
Pulse Decomposition Algorithm and Intra-Arterial
Catheters in ICU Patients
Introduction
The object of the work presented here was to validate a new approach to tracking blood pressure that is
based on the pulse analysis of the peripheral arterial pressure pulse. The approach, referred to as the
Pulse Decomposition Analysis (PDA) model, goes beyond traditional pulse analysis by invoking a
physical model that comprehensively links the components of the peripheral pressure pulse
envelope with two reflection sites in the centralarteries. The first reflection site is the juncture
between thoracic and abdominal aorta, which is marked by a significant decrease in diameter and a
change in elasticity. The second site arises from the juncture between abdominal aorta and the common
iliac arteries.
The PDA model integrates and goes beyond the findings of a number of studies that have confirmed
the existence of the two reflection sites. [Kriz 2008,
Latham 1985] A consequence of these reflection sites are two reflected arterial pressure pulses, referred
to as component pulses, which counter-propagate to the direction of the single arterial pressure pulse,
due to left ventricular contraction, that gave rise to them. The scenario, sketched in Figure 1, has been
described in detail elsewhere. [Baruch 2011] In the arterial periphery, and specifically at the radial or
digital arteries, these reflected pulses, the renal reflection pulse (P2, also known as the second systolic
pulse) and the iliac reflection pulse (P3), arrive with distinct time delays. In the case of P2 the delay is
typically between 70 and 140 milliseconds, in the case of P3 between 180 to 450 milliseconds.
Quantification of physiological parameters is accomplished by extracting pertinent component pulse
parameters. In the case of the beat-by-beat tracking of blood pressure the PDA model’s predictions and
previous experimental studies have shown that two pulse parameters are of particular importance. The
ratio of the amplitude of the renal reflection pulse (P2) to that of the primary systolic pulse (P1) tracks
changes in beat-by-beat systolic pressure. The time difference between the arrival of the primary
systolic (P1) pulse and the iliac reflection (P3) pulse, referred to as T13, tracks changes in arterial pulse
pressure.
Patients and Methods
In these experiments, approved by the University of Virginia Medical Center Review Board, the arterial
blood pressures of patients (23 m/11 f, mean age: 44.05 y, SD: 13.9 y, mean height: 173.3 cm, SD: 9.4
cm, mean weight: 95.3 kg, SD: 27.4 kg) hospitalized in the University of Virginia Medical Intensive Care
Unit (MICU) were monitored using radial intra-arterial catheters, while the CareTaker system collected
pulse line shapes at the lower phalange of the thumb. The overlap recording sessions with both
monitoring systems were scheduled for four hours but were frequently shorter because of medical
procedures. BedMaster (Excel Medical, Jupiter, FL) hardware and software was used to digitize and
record intra-arterial waveform data from the GE Unity network at a sample rate of 240 Hz.
Consent for data collection was obtained for 60 patients, and 34 successful data overlaps between
arterial catheter and CareTaker were obtained. Eleven arterial data sets were lost because of a
programming error in the BedMaster software, causing data to be overwritten when the overall arterial
catheter recording session extended beyond one day after the CareTaker/arterial catheter overlap
recording window. In 4 cases the BedMaster system was found to have been inoperative during the
recording window. In 4 cases the arterial catheter recordings did not include the overlap recording
window for unknown reasons, while in 4 additional cases the arterial catheter failed. Two cases involved
such substantial movement artifacts due to movement, extubation etc. that neither system was able to
obtain valid recordings. In one case the CareTaker device became accidently disconnected early in the
session.
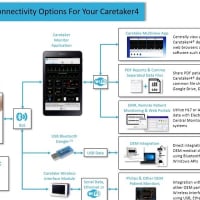
A. CareTaker Device and PDA model
The hardware platform, which is the Care-Taker device (Empirical Technologies Corporation,
Charlottesville, Virginia) the model, and the algorithm implementation have been described in detail
elsewhere [Baruch].
B. Statistical analysis
We present regression coefficients and linear fits between arterial catheter blood pressures and the PDA
parameters P2P1 and T13 for an individual patient, histogram distributions of the slopes of the linear fits
for individual patients, as well as overall linear fit-based comparisons between central catheter blood
pressures and blood pressures obtained from the PDA parameters using a single set of conversion
constants. Bland-Altman comparisons of the two sets of blood pressures are also provided.
C. Data Inclusion
Data were excluded from analysis on the following basis:
In the case of the arterial catheter data the criteria for exclusion were as follows: A. visual inspection of
the data was used to identify sections of obvious catheter failure, characterized by either continuous or
pervasive intermittent analog/digital readings of -/+32768. B. sections contaminated by excessive
motion artifact were identified as such if the peak detection algorithm was no longer able to identify
FactorTime (Seconds)
heart beats, as evidenced by inspection of the resulting implausible and discontinuous inter-beat
interval spectrum.
In the case of the CareTaker data a Fourier spectral analysis approach was used to establish a
signal/noise factor (SNF) to identify poor quality data sections. To this end the standard deviations and
integrated amplitudes of different spectral bands were calculated. The band associated with the
physiological signal was chosen from 1-10 Hz, based on data by the authors and published results by
others. The signal strength associated with this band was compared with those of the 100-250 Hz
frequency band, which is subject to ambient noise but contains no physiologically relevant signal. The
spectrogram (top graph) displayed in figure 10 provides a motivation. Data sections characterized by low
noise feature low high-frequency spectral amplitudes and high low-frequency spectral amplitudes as
well as “structured” physiological bands, i.e. significant amplitude variations between the harmonic
bands. This motivates the analytical form of the SNF parameter, which is established by taking the ratio
A-line DiastoleTime (Seconds)
of the standard deviation of the 1-10 Hz band to the product of the integrated band strengths of the 1-
10 Hz and 100-250 frequency bands. The bottom graph of Figure 2 displays the SNF parameter for the
raw CareTaker data presented in the center graph of Figure 2. Data sections with an SNF below 80 were
excluded from the analysis.
Results
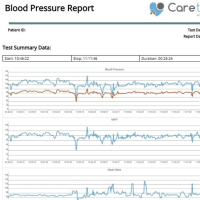
The overlap of the CareTaker data streams and the central catheter data streams was established, after
an initial alignment based on data collection systems clocks, by matching time-based inter-beat interval
spectra obtained via pulse detection obtained from both data streams. Figure 3 presents an example of
such an overlap for patient 21. The figure presents both an overall overlay of the data streams, as well
as a 70 second expanded section.
The linear model used to perform the conversion of the P2P1 parameters to systolic blood pressure for
patient 21 was (140 × P2P1 (unitless ratio) + 59.2), while the corresponding linear conversion for the T13
parameter to pulse pressure was (0.1 × T13 (milliseconds) + 13.6). Both the offsets and the slope factors
were patient-specific and obtained by chi^2 minimization of the fit of both data streams. The details of
obtaining the slope factor and the offset for individual patients, as well as the physiological relevance of
the slope factor regarding arterial stiffness, are discussed later.
In figures 9 and 10 we present the correlation and Bland-Altman results for the interbeat interval data
for patient 21, which was presented in Figure 2. The data presented in the Bland-Altman plot of figure 9
demonstrates the resolution limits of the data streams, which presents itself as diagonally-running
striations that are visible in the data. Had the data rate in both data streams been equal, the striations
would run at 45 degrees. In the case of the CareTaker data, the acquisition rate was 500 Hz, or a data
point spacing of 2.0 milliseconds, while the catheter-based data was collected at 240 Hz, corresponding
to a data point spacing of 4.16 milliseconds. Consequently the slope of the striations is 0.48, the ratio of
lower to higher data acquisition rate.
Overall Blood Pressure Results
The overall results of the study are presented as blood pressure correlations and Bland-Altman graphs in
figures 11 through 14. The data comparisons are based on two-second averages of 40-minute sections
from each patient. This approach is an established procedure that has been used in previous
presentations of comparative blood pressure data by others. 1 One important benefit of this approach is
that it gives equal weight to the data set of each patient
1 Martina JR et. al., Noninvasive continuous arterial blood pressure monitoring with Nexfin, Anesthesiology. 2012
May;116(5):1092-103.
Average Inter-beat Interval (Seconds))
mean: -0.056 millisecondsSD: 6.0 milliseconds
larger standard deviation observed here is affected by two factors: 1. the comparatively low sampling
rate of the catheter signal, 240 Hz corresponding to 4.2 milliseconds, and 2. the significantly broader
structure of the blood pressure pulse compared to the EKG signal. The first limits the temporal
resolution of peak detection, while the second limits the threshold accuracy with which a given peak can
be detected relative to other peaks, likewise introducing uncertainty into the temporal accuracy.
Pulse Decomposition Algorithm and Intra-Arterial
Catheters in ICU Patients
Introduction
The object of the work presented here was to validate a new approach to tracking blood pressure that is
based on the pulse analysis of the peripheral arterial pressure pulse. The approach, referred to as the
Pulse Decomposition Analysis (PDA) model, goes beyond traditional pulse analysis by invoking a
physical model that comprehensively links the components of the peripheral pressure pulse
envelope with two reflection sites in the centralarteries. The first reflection site is the juncture
between thoracic and abdominal aorta, which is marked by a significant decrease in diameter and a
change in elasticity. The second site arises from the juncture between abdominal aorta and the common
iliac arteries.
The PDA model integrates and goes beyond the findings of a number of studies that have confirmed
the existence of the two reflection sites. [Kriz 2008,
Latham 1985] A consequence of these reflection sites are two reflected arterial pressure pulses, referred
to as component pulses, which counter-propagate to the direction of the single arterial pressure pulse,
due to left ventricular contraction, that gave rise to them. The scenario, sketched in Figure 1, has been
described in detail elsewhere. [Baruch 2011] In the arterial periphery, and specifically at the radial or
digital arteries, these reflected pulses, the renal reflection pulse (P2, also known as the second systolic
pulse) and the iliac reflection pulse (P3), arrive with distinct time delays. In the case of P2 the delay is
typically between 70 and 140 milliseconds, in the case of P3 between 180 to 450 milliseconds.
Quantification of physiological parameters is accomplished by extracting pertinent component pulse
parameters. In the case of the beat-by-beat tracking of blood pressure the PDA model’s predictions and
previous experimental studies have shown that two pulse parameters are of particular importance. The
ratio of the amplitude of the renal reflection pulse (P2) to that of the primary systolic pulse (P1) tracks
changes in beat-by-beat systolic pressure. The time difference between the arrival of the primary
systolic (P1) pulse and the iliac reflection (P3) pulse, referred to as T13, tracks changes in arterial pulse
pressure.
Patients and Methods
In these experiments, approved by the University of Virginia Medical Center Review Board, the arterial
blood pressures of patients (23 m/11 f, mean age: 44.05 y, SD: 13.9 y, mean height: 173.3 cm, SD: 9.4
cm, mean weight: 95.3 kg, SD: 27.4 kg) hospitalized in the University of Virginia Medical Intensive Care
Unit (MICU) were monitored using radial intra-arterial catheters, while the CareTaker system collected
pulse line shapes at the lower phalange of the thumb. The overlap recording sessions with both
monitoring systems were scheduled for four hours but were frequently shorter because of medical
procedures. BedMaster (Excel Medical, Jupiter, FL) hardware and software was used to digitize and
record intra-arterial waveform data from the GE Unity network at a sample rate of 240 Hz.
Consent for data collection was obtained for 60 patients, and 34 successful data overlaps between
arterial catheter and CareTaker were obtained. Eleven arterial data sets were lost because of a
programming error in the BedMaster software, causing data to be overwritten when the overall arterial
catheter recording session extended beyond one day after the CareTaker/arterial catheter overlap
recording window. In 4 cases the BedMaster system was found to have been inoperative during the
recording window. In 4 cases the arterial catheter recordings did not include the overlap recording
window for unknown reasons, while in 4 additional cases the arterial catheter failed. Two cases involved
such substantial movement artifacts due to movement, extubation etc. that neither system was able to
obtain valid recordings. In one case the CareTaker device became accidently disconnected early in the
session.
A. CareTaker Device and PDA model
The hardware platform, which is the Care-Taker device (Empirical Technologies Corporation,
Charlottesville, Virginia) the model, and the algorithm implementation have been described in detail
elsewhere [Baruch].
B. Statistical analysis
We present regression coefficients and linear fits between arterial catheter blood pressures and the PDA
parameters P2P1 and T13 for an individual patient, histogram distributions of the slopes of the linear fits
for individual patients, as well as overall linear fit-based comparisons between central catheter blood
pressures and blood pressures obtained from the PDA parameters using a single set of conversion
constants. Bland-Altman comparisons of the two sets of blood pressures are also provided.
C. Data Inclusion
Data were excluded from analysis on the following basis:
In the case of the arterial catheter data the criteria for exclusion were as follows: A. visual inspection of
the data was used to identify sections of obvious catheter failure, characterized by either continuous or
pervasive intermittent analog/digital readings of -/+32768. B. sections contaminated by excessive
motion artifact were identified as such if the peak detection algorithm was no longer able to identify
FactorTime (Seconds)
heart beats, as evidenced by inspection of the resulting implausible and discontinuous inter-beat
interval spectrum.
In the case of the CareTaker data a Fourier spectral analysis approach was used to establish a
signal/noise factor (SNF) to identify poor quality data sections. To this end the standard deviations and
integrated amplitudes of different spectral bands were calculated. The band associated with the
physiological signal was chosen from 1-10 Hz, based on data by the authors and published results by
others. The signal strength associated with this band was compared with those of the 100-250 Hz
frequency band, which is subject to ambient noise but contains no physiologically relevant signal. The
spectrogram (top graph) displayed in figure 10 provides a motivation. Data sections characterized by low
noise feature low high-frequency spectral amplitudes and high low-frequency spectral amplitudes as
well as “structured” physiological bands, i.e. significant amplitude variations between the harmonic
bands. This motivates the analytical form of the SNF parameter, which is established by taking the ratio
A-line DiastoleTime (Seconds)
of the standard deviation of the 1-10 Hz band to the product of the integrated band strengths of the 1-
10 Hz and 100-250 frequency bands. The bottom graph of Figure 2 displays the SNF parameter for the
raw CareTaker data presented in the center graph of Figure 2. Data sections with an SNF below 80 were
excluded from the analysis.
Results
The overlap of the CareTaker data streams and the central catheter data streams was established, after
an initial alignment based on data collection systems clocks, by matching time-based inter-beat interval
spectra obtained via pulse detection obtained from both data streams. Figure 3 presents an example of
such an overlap for patient 21. The figure presents both an overall overlay of the data streams, as well
as a 70 second expanded section.
The linear model used to perform the conversion of the P2P1 parameters to systolic blood pressure for
patient 21 was (140 × P2P1 (unitless ratio) + 59.2), while the corresponding linear conversion for the T13
parameter to pulse pressure was (0.1 × T13 (milliseconds) + 13.6). Both the offsets and the slope factors
were patient-specific and obtained by chi^2 minimization of the fit of both data streams. The details of
obtaining the slope factor and the offset for individual patients, as well as the physiological relevance of
the slope factor regarding arterial stiffness, are discussed later.
In figures 9 and 10 we present the correlation and Bland-Altman results for the interbeat interval data
for patient 21, which was presented in Figure 2. The data presented in the Bland-Altman plot of figure 9
demonstrates the resolution limits of the data streams, which presents itself as diagonally-running
striations that are visible in the data. Had the data rate in both data streams been equal, the striations
would run at 45 degrees. In the case of the CareTaker data, the acquisition rate was 500 Hz, or a data
point spacing of 2.0 milliseconds, while the catheter-based data was collected at 240 Hz, corresponding
to a data point spacing of 4.16 milliseconds. Consequently the slope of the striations is 0.48, the ratio of
lower to higher data acquisition rate.
Overall Blood Pressure Results
The overall results of the study are presented as blood pressure correlations and Bland-Altman graphs in
figures 11 through 14. The data comparisons are based on two-second averages of 40-minute sections
from each patient. This approach is an established procedure that has been used in previous
presentations of comparative blood pressure data by others. 1 One important benefit of this approach is
that it gives equal weight to the data set of each patient
1 Martina JR et. al., Noninvasive continuous arterial blood pressure monitoring with Nexfin, Anesthesiology. 2012
May;116(5):1092-103.
Average Inter-beat Interval (Seconds))
mean: -0.056 millisecondsSD: 6.0 milliseconds
larger standard deviation observed here is affected by two factors: 1. the comparatively low sampling
rate of the catheter signal, 240 Hz corresponding to 4.2 milliseconds, and 2. the significantly broader
structure of the blood pressure pulse compared to the EKG signal. The first limits the temporal
resolution of peak detection, while the second limits the threshold accuracy with which a given peak can
be detected relative to other peaks, likewise introducing uncertainty into the temporal accuracy.