When I work on patients with pectus excavatum, I incise the skin of their chests in different fashions. For some, I make incisions similar to the icon of Mercedes (a German automobile maker) (Figure 1); for others, I incise across the chest, with an incision line looking like a flying bird (Figure 2).

Figure 1

Figure 2
I decide the skin incision’s fashion for each patient by referring to the structure of his/her thorax. My basic principles are: 1. Sever every bone hindering elevation of the concave part of the chest wall; 2. Minimize the length of skin incision.
For instance, Figure 3 is a graphic image of the thorax of the patient in Figure 1. Before the operation, I explained, showing Figure 3 to the patient, as follows: “Your sternum presents deformity. It bends toward the back at point A. Therefore, I need to sever your sternum to straighten it at Point A. Similarly, the ribs distort inwards at the points indicated with arrows. Therefore, the ribs need to be severed at these points. Therefore, I make a Mercedes-type skin incision to expose all the points.”

Figure 3

Figure 4
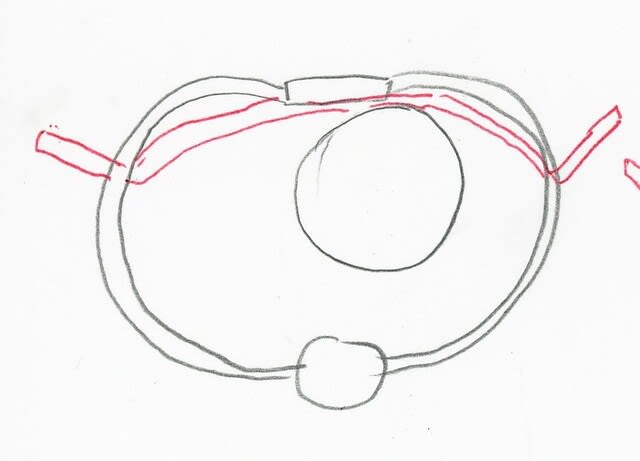
Almost all patients are happy with such explanation. However, I recently have found another way of explanation, which I think is more persuasive. I tell the patient to draw a circle on his/her chest wall around the area that he/she thinks sagged in. Then I let him/her draw a line corresponding to the circle (Figure 4). Thereafter, I ask: “We need to elevate the area inside the circle, right?” The answer: “Right.”
I ask further, “We need to incise your skin to expose the chest wall and sever ribs on the circle. Can you describe an incision line on your chest wall that enables our access to the bones? You can minimize the skin incision. I’ll incise your skin as you instruct, as long as it enables my access to the chest wall.” The patient struggles to find the best answer to this geometrical question, and eventually draws a circle like in Figure 5. Through this sort of explanation, the patient can personally understand that the design I provide is the best solution.

Figure 5
The size of the circle can differ depending on the area of deformity. The patient in Figure 5 had a large concavity on his chest wall. Since the deformity extended to almost all of his thorax, I had to expose the entire chest wall to correct it, which required the skin incision in Figure 6. Although we made a long incision on the chest wall of the patient, we sutured the wound with greatest care, so the scar would gradually become inconspicuous. Figure 7 shows the condition of the scar two years after the operation.

Figure 6

Figure 7